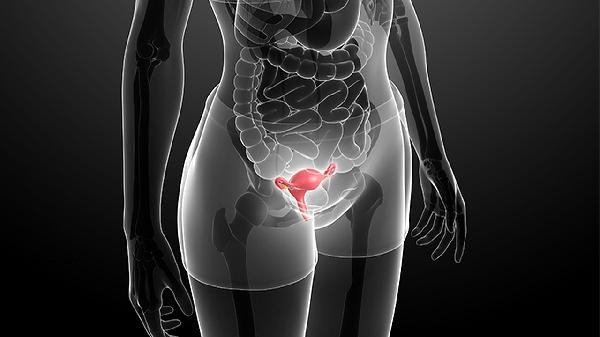
Getting vaccinated with HPV 9-valent vaccine may still lead to cervical cancer, but the probability is significantly reduced. The HPV nine valent vaccine can prevent about 90% of high-risk HPV infections related to cervical cancer, but it cannot cover all carcinogenic types, and regular screening is still required after vaccination. The HPV nine valent vaccine targets seven high-risk types, namely HPV16, 18, 31, 33, 45, 52, and 58, as well as two low-risk types, HPV6 and 11, which together account for approximately 90% of cervical cancer cases. Vaccines effectively block the above-mentioned types of infections by stimulating immune responses to produce antibodies, thereby significantly reducing the risk of cancer. However, there are still a few cases of cervical cancer associated with uncovered HPV types such as HPV35, 39, 51, or caused by persistent infection with viruses that have not been completely cleared by vaccines. In addition, vaccines have no therapeutic effect on HPV infections that existed before vaccination. If the infection is not cleared by the immune system, it may still progress to precancerous lesions. The protective effect after vaccination is influenced by individual differences. People with low immune function may have insufficient antibody production, and factors such as smoking and long-term oral contraceptives can also increase the risk of cervical cancer. In rare cases, cervical cancer may be related to non HPV factors such as genetic or environmental exposure to carcinogens, which vaccines cannot prevent. Clinical data shows that the incidence of cervical cancer has significantly decreased after vaccination, but there are still sporadic case reports, mostly related to failure to screen in a timely manner or incomplete full vaccination.
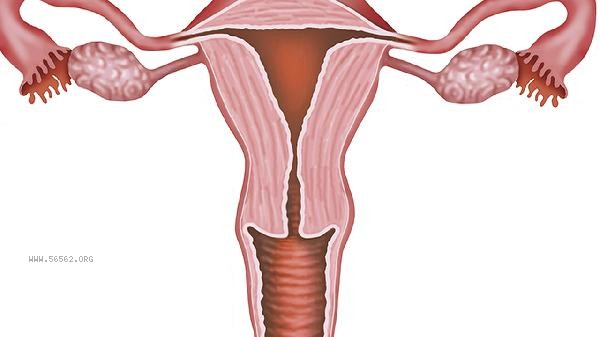
It is recommended to undergo cervical TCT combined with HPV screening every 3-5 years after vaccination, and promptly address any abnormalities found. Maintaining a single sexual partner, using condoms, and quitting smoking can further reduce the risk. If there are symptoms such as abnormal vaginal bleeding and discharge, regardless of vaccination history, medical examination is necessary.










Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!