High bilirubin in children may be related to genetic metabolic abnormalities, breast milk jaundice, infectious diseases, hepatobiliary diseases, hemolytic diseases and other factors. Elevated bilirubin levels are usually manifested as symptoms such as yellowing of the skin, darkening of urine color, and decreased appetite. It is necessary to combine laboratory tests to determine the cause.
1. Genetic metabolic abnormalities
Hereditary hyperbilirubinemia such as Gilbert syndrome, Krieger Nagel syndrome, etc. can lead to bilirubin metabolism disorders. This type of disease is often associated with UGT1A1 gene mutations, manifested as an increase in unconjugated bilirubin. The child may have mild jaundice, but the general condition is good. Regular monitoring of liver function is necessary, and genetic testing may be performed if necessary. Clinically, phenobarbital tablets can be used according to medical advice to promote bilirubin metabolism, and in severe cases, phototherapy intervention is required.
2. Breast milk jaundice
Excessive activity of β - glucuronidase in breast milk may cause breast milk jaundice, which is more common in healthy full-term infants 1-2 weeks after birth. The bilirubin level usually does not exceed 15mg/dL, and jaundice can significantly subside after stopping breastfeeding for 3 days. This situation does not require special treatment. It is recommended that parents continue breastfeeding and strengthen sunlight exposure. If necessary, use Yinzhihuang oral solution to assist in jaundice reduction.
3. infectious diseases
Newborn sepsis, cytomegalovirus infection, etc. can cause liver cell damage, leading to simultaneous increase of conjugated bilirubin and transaminase. Children with jaundice often present with symptoms of infection such as fever and poor response, which can be confirmed by blood culture and virological examination. Treatment requires the use of injectable ceftriaxone sodium or ganciclovir injection targeting the pathogen, combined with liver protective drugs such as compound glycyrrhizin tablets.
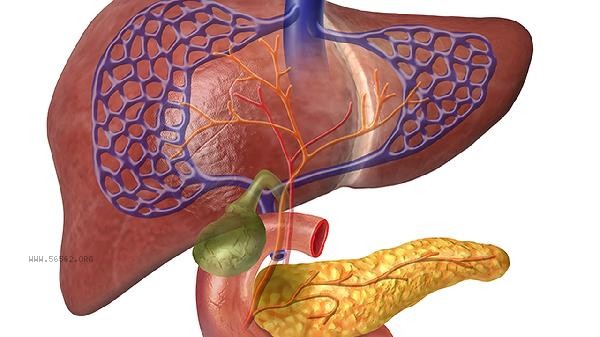
4. Diseases of the liver and gallbladder system
Biliary atresia, infantile hepatitis syndrome, and other diseases can lead to bile excretion disorders, manifested as significantly increased clay colored feces and direct bilirubin. Ultrasound examination shows abnormal development of bile ducts, and liver biopsy is helpful for differential diagnosis. Early diagnosis requires Gexi surgery or liver transplantation, and medication treatment can use ursodeoxycholic acid capsules to improve bile stasis.
5. Hemolytic diseases
ABO hemolytic disease, G6PD deficiency, etc. can cause extensive destruction of red blood cells, leading to a sharp increase in indirect bilirubin. The jaundice in the child appears early and progresses rapidly, which may be accompanied by anemia and hepatosplenomegaly. Emergency situations require blood exchange treatment. For mild cases, human serum albumin injection combined with blue light irradiation can be used, and sodium bicarbonate tablets can be taken orally to alkalize urine.
Parents should promptly measure the transcutaneous bilirubin level and record the range of jaundice and changes in the color of urine and feces when their children's skin is yellow stained. Ensure adequate feeding to promote bilirubin excretion and avoid the use of drugs such as sulfonamides that may induce hemolysis. If jaundice persists for 2 weeks or is accompanied by symptoms such as mental fatigue and refusal to breastfeed, immediate medical attention should be sought for liver function, blood routine, and imaging examinations. Pay attention to observing the degree of scleral yellowing and urine color in daily life, and regularly follow up on changes in bilirubin levels.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!