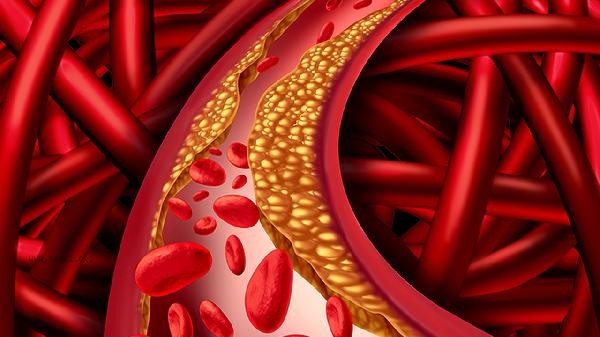
Erythrocytosis can be improved through methods such as bloodletting therapy, medication treatment, lifestyle adjustments, etiological treatment, and regular monitoring. This disease may be caused by factors such as altitude sickness, chronic hypoxia, myeloproliferative disorders, gene mutations, tumors, etc.

1. Bloodletting therapy:
Venous bloodletting is the first-line treatment for primary erythrocytosis, which reduces blood volume and viscosity by regularly drawing 300-500ml of whole blood. In the initial stage of treatment, 1-2 times a week are required, and the interval can be extended after the hematocrit drops below 45%. It is necessary to cooperate with fluid replacement to prevent hypotension, while monitoring ferritin levels to prevent iron deficiency anemia.
2. Drug therapy:
Hydroxyurea can inhibit bone marrow hematopoietic function and is suitable for patients with high-risk factors for thrombosis; Interferon alpha can regulate immunity and inhibit abnormal hematopoiesis; Lukotinib has a significant effect on patients with JAK2 gene mutations. During the medication period, blood routine tests should be conducted weekly to observe changes in white blood cells and platelets, and to be alert to side effects such as bone marrow suppression.
3. Lifestyle adjustment:
Daily water intake should reach 2000ml or more to reduce blood viscosity. Quitting smoking can improve endothelial function and avoid high-altitude travel to prevent hypoxia stimulation. It is recommended to engage in aerobic exercises such as swimming and brisk walking, but it is important to avoid intense exercise that may trigger blood clots. Diet should control red meat intake and increase anticoagulant foods such as deep-sea fish.
4. Etiological treatment:
Secondary erythrocytosis requires targeted intervention for the primary disease. Patients with chronic obstructive pulmonary disease require long-term oxygen therapy. Sleep apnea syndrome should be treated with a ventilator. Tumors such as kidney cancer require surgical resection. If patients with polycythemia vera have complications of splenomegaly, splenic radiotherapy or splenectomy may be considered.
5. Regular monitoring:
Blood routine, JAK2 gene, and bone marrow biopsy should be rechecked every 3 months to monitor the progression of the disease. Focus on observing thrombotic prodromal symptoms such as headache and dizziness, and regularly conduct fundus examinations to evaluate microcirculation status. Patients with combined hypertension need to monitor their blood pressure daily and control the target value below 130/80mmHg. Patients with polycythemia should maintain a light diet, consume more foods such as black fungus and onions that have anti platelet aggregation effects, and limit high purine diets such as animal organs. It is recommended to choose soothing exercises such as yoga and Tai Chi, and avoid high-temperature environments such as saunas. Raising the head of the bed during sleep can improve nighttime breathing, and daily use of elastic socks can prevent lower limb venous thrombosis. Perform echocardiography every six months to evaluate cardiac load. Women of childbearing age should use contraception until their condition stabilizes, and carry a disease description card with them when going out for emergency needs.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!