gastrointestinal bleeding can indeed cause a decrease in blood pressure, and in severe cases, it may lead to shock, requiring timely medical attention. The main reason for decreased blood pressure caused by gastrointestinal bleeding is excessive blood loss, resulting in a decrease in circulating blood volume and thus affecting blood pressure stability. The treatment methods include hemostasis, blood volume supplementation, drug therapy, and surgical intervention.
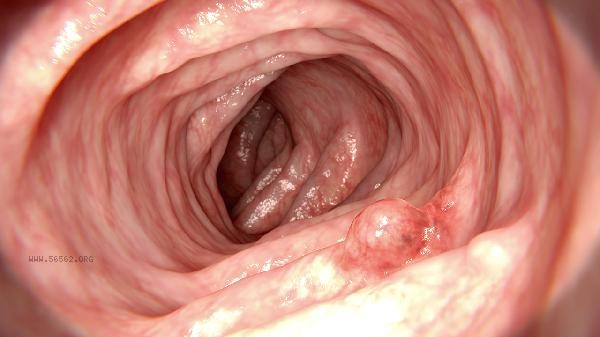
1. Excessive blood loss is the direct cause of decreased blood pressure caused by gastrointestinal bleeding. Gastrointestinal bleeding includes upper gastrointestinal bleeding and lower gastrointestinal bleeding. Common causes include gastric ulcer, duodenal ulcer, esophageal varices, gastric cancer, colon cancer, etc. When the amount of bleeding is large, blood loss can lead to a decrease in circulating blood volume, a decrease in the heart's pumping ability, and ultimately a decrease in blood pressure. In severe cases, shock symptoms may occur, such as pale complexion, cold sweat, and increased heart rate. Hemostasis is the primary measure for treating gastrointestinal bleeding. Endoscopic hemostasis is a commonly used method, which involves finding the bleeding point through endoscopy and using methods such as electrocoagulation, drug injection, or occlusion of blood vessels to stop the bleeding. Drug therapy is also an important means, and commonly used drugs include proton pump inhibitors such as omeprazole, H2 receptor antagonists such as ranitidine, and hemostatic drugs such as tranexamic acid. For severe bleeding, blood transfusion may be necessary to replenish blood volume and maintain stable blood pressure.
3. Supplementing blood volume is the key to stabilizing blood pressure. In the early stages of bleeding, physiological saline or lactate Ringer's solution can be supplemented through intravenous infusion to maintain circulating blood volume. For patients with significant blood loss, it may be necessary to administer red blood cell suspension or plasma to restore blood oxygen carrying capacity and coagulation function. During the treatment process, it is necessary to closely monitor blood pressure, heart rate, and urine output, and adjust the treatment plan in a timely manner.

4. Surgical intervention is suitable for severe cases where drug therapy and endoscopic hemostasis are ineffective. Surgical methods include subtotal gastrectomy, esophageal vein ligation, and colectomy. Surgery can completely stop bleeding, but the risk is high and should be carefully selected according to the specific situation of the patient. Postoperative monitoring of blood pressure and bleeding is necessary to prevent complications. The decrease in blood pressure caused by gastrointestinal bleeding is a critical situation that requires timely medical attention and comprehensive treatment measures. By stopping bleeding, supplementing blood volume, medication treatment, and surgical intervention, bleeding can be effectively controlled, blood pressure can be stabilized, and serious consequences such as shock can be prevented. Patients should pay attention to dietary regulation in daily life, avoid stimulating foods, undergo regular physical examinations, detect and treat digestive diseases early, and reduce the risk of bleeding.










Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!