Untreated pulmonary embolism may lead to pulmonary hypertension, right heart failure, and even sudden death. The consequences of not intervening in a timely manner mainly include thrombus enlargement, pulmonary tissue ischemic necrosis, chronic pulmonary hypertension, compensatory damage to cardiac function, and multi organ hypoxic lesions.
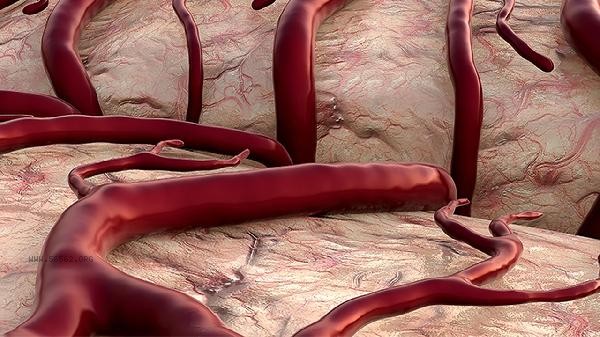
1. Thrombosis enlargement:
Initial embolism may only affect local small arteries, but when left untreated, the thrombus will continue to grow or shed new clots. Platelet aggregation and activation of the coagulation system form a positive feedback loop, leading to the expansion of embolism from subsegmental pulmonary arteries to lobular arteries. Hemodynamic abnormalities occur when the pulmonary vascular cross-sectional area decreases by more than 30%.
2. Formation of pulmonary infarction:
Obstruction of distal lung tissue leads to hemorrhagic necrosis due to ischemia, which is more common in patients with pre-existing heart and lung diseases. The destruction of alveolar walls releases inflammatory mediators, and clinical manifestations include sudden chest pain, hemoptysis, and pleural effusion. The chest X-ray shows a wedge-shaped shadow pointing towards the hilum of the lung, and the necrotic area may become fibrotic in the later stage.
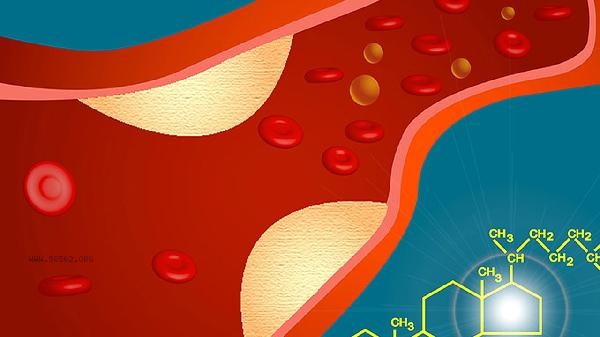
3. Chronic pulmonary arterial hypertension:
Repeated embolism leads to progressive reduction of pulmonary vascular bed and sustained increase in vascular resistance. Increased right ventricular afterload leads to ventricular wall hypertrophy, and ultrasound shows pulmonary artery systolic pressure>40mmHg. The patient's dyspnea worsened after physical activity, and the jugular vein became engorged, eventually progressing to irreversible pulmonary heart disease.
4. Right heart failure:
Persistent pulmonary arterial hypertension leads to decreased right ventricular dilation and contraction function, resulting in signs of systemic congestion. Lower limb edema, positive hepatic jugular venous reflux sign, and ascites indicate decompensated phase, with significantly elevated BNP levels. The electrocardiogram shows changes such as QR waves in lead V1 and complete right bundle branch block.
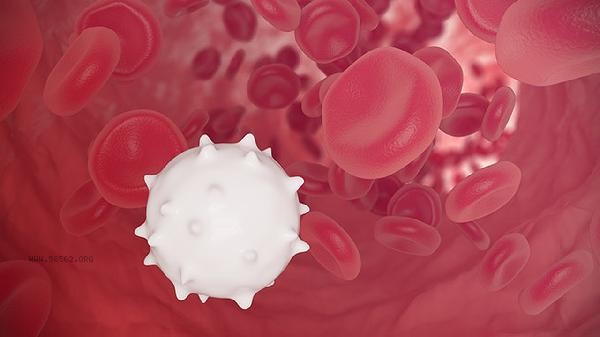
5. Multiple organ hypoxia injury:
Decreased cardiac output leads to insufficient systemic perfusion, cerebral hypoxia causes confusion, and renal ischemia leads to oliguric renal failure. In severe cases, sudden death may occur due to malignant arrhythmia or cardiogenic shock. Autopsy shows extensive dissolution and necrosis of myocardial cells in the free wall of the right ventricle. After being diagnosed with pulmonary embolism, anticoagulant therapy should be initiated immediately. The combination of low molecular weight heparin and warfarin can reduce the risk of recurrence. It is recommended to wear medical elastic socks during the recovery period to prevent deep vein thrombosis in the lower limbs, and to perform ankle pump exercises daily to promote blood circulation. Choose high protein, low-fat and easily digestible foods for diet, limit sodium intake to reduce heart load. Three months later, a follow-up echocardiogram will be performed to evaluate pulmonary artery pressure. Long term follow-up will require monitoring of D-dimer and coagulation function. When there is a progressive decrease in activity endurance or symptoms of hemoptysis, timely follow-up should be sought.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!