Direct increase in eosinophil count can be intervened through anti allergic therapy, parasite screening, medication adjustment, inflammation control, and blood disease screening. It is usually caused by allergic reactions, parasitic infections, drug side effects, chronic inflammation, or blood system diseases.

1. Anti allergic therapy:
Allergic rhinitis, asthma and other diseases are prone to causing eosinophilia. Antihistamines such as loratadine and cetirizine can alleviate symptoms, and in severe cases, inhaled corticosteroids should be used in combination. Allergen testing helps identify triggers and avoid contact with common allergens such as pollen and dust mites.
2. Parasite screening:
Intestinal parasitic infections such as roundworms and hookworms are common causes. Fecal egg examination can confirm the diagnosis, and anthelmintics such as albendazole and benzimidazole can effectively treat it. Individuals with travel history or raw food habits in epidemic areas should be screened with special attention, especially when accompanied by symptoms of abdominal pain and weight loss.
3. Drug adjustment:
Penicillin and cephalosporin antibiotics may cause drug-induced eosinophilia. Need to investigate recent medication history and switch to alternative medications under the guidance of a doctor. Usually, the indicators can return to normal 2-4 weeks after discontinuation of medication, and changes in blood routine should be monitored during this period. 4. Inflammation control: Chronic inflammatory diseases such as rheumatoid arthritis and eosinophilic granulomas are often accompanied by elevated indicators. Non steroidal anti-inflammatory drugs can alleviate symptoms, and in severe cases, immunosuppressants should be used. Inflammatory indicators such as C-reactive protein and erythrocyte sedimentation rate assist in diagnosis.
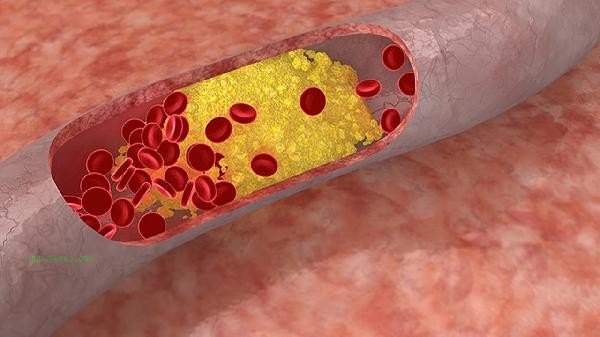
5. Blood disease screening:
Eosinophilic leukemia, myeloproliferative neoplasms, etc. require bone marrow puncture for diagnosis. When immature cells are seen on peripheral blood smears, accompanied by persistent fever or hepatosplenomegaly, prompt medical attention should be sought from the hematology department. Genetic testing can identify specific chromosomal abnormalities.
It is necessary to maintain a light diet in daily life, increase the intake of citrus fruits rich in vitamin C, and avoid spicy and stimulating foods. Moderate aerobic exercise such as brisk walking and swimming can enhance immunity, but individuals with allergies should avoid outdoor activities during the pollen season. Regularly check the blood routine. If the absolute value of eosinophils continues to be greater than 1.5 × 10 ⁹/L or accompanied by symptoms such as weight loss and lymph node enlargement, it is recommended to complete further examinations such as bone marrow biopsy. Pay attention to cleaning bedding at home to reduce the growth of dust mites, and thoroughly wash hands after handling raw food to prevent parasitic infections.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!