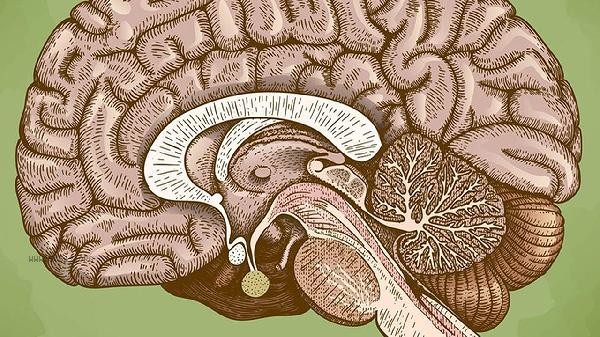
The loss of memory in the brain may be caused by diseases such as Alzheimer's disease, transient global amnesia, traumatic brain injury, stroke, encephalitis, etc. The main manifestations of memory impairment include short-term memory loss, long-term memory impairment, episodic memory loss, semantic memory impairment, and procedural memory abnormalities. It is recommended to seek medical examination in a timely manner, clarify the cause, and receive targeted treatment.
1. Alzheimer's disease
Alzheimer's disease is the most common neurodegenerative disease, mainly characterized by progressive memory loss and cognitive decline. Early symptoms are mostly recent memory impairment, and as the condition progresses, symptoms such as impaired orientation and language function may appear. This disease is related to the deposition of beta amyloid protein and neurofibrillary tangles, and can be diagnosed through cerebrospinal fluid testing and imaging examinations. The therapeutic drugs include acetylcholinesterase inhibitors such as donepezil, rivastigmine, and memantine.
2. Transient global amnesia
Transient global amnesia is characterized by sudden anterograde forgetting, in which patients are unable to form new memories but retain their own identity and long-term memory. The attack usually lasts for several hours and may be related to temporary ischemia in the temporal lobe and hippocampus. This disease is self limiting, and most patients fully recover within 24 hours, but it is necessary to rule out causes such as epilepsy and cerebrovascular disease. Preventive measures include controlling hypertension, diabetes and other basic diseases.
3. Traumatic brain injury
Memory impairment caused by traumatic brain injury is closely related to the site of injury, commonly occurring in the frontal and temporal lobes. Mild traumatic brain injury may result in transient memory loss, while severe injury can lead to persistent amnesia syndrome. Clinical manifestations include retrograde amnesia, anterograde amnesia, and fictitious symptoms. rehabilitation therapy includes non pharmacological interventions such as cognitive training and memory strategy training. In severe cases, drugs that improve brain metabolism, such as phosphatidylcholine, may be considered.

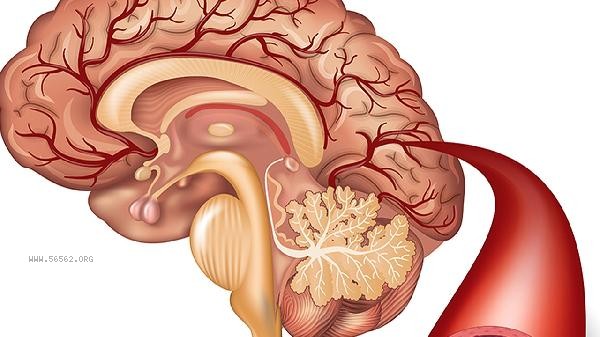
4. Stroke
Post stroke memory impairment is more common in memory related areas such as thalamus and hippocampus infarction. Patients may exhibit symptoms such as impaired working memory and episodic memory impairment, often accompanied by other neurological deficits. The acute phase treatment mainly involves thrombolysis or thrombectomy, while the recovery phase requires systematic cognitive rehabilitation training. Preventive measures include controlling risk factors for cerebrovascular disease such as blood pressure and blood lipids.
5. Encephalitis
Both viral and autoimmune encephalitis can impair memory function, especially herpes simplex virus encephalitis which often affects the temporal lobe. In addition to memory impairment, patients may also have symptoms such as abnormal mental behavior and epileptic seizures. Diagnosis relies on cerebrospinal fluid examination and imaging findings, while treatment requires the use of antiviral drugs or immunosuppressants based on the cause. Early intervention can help improve prognosis. For patients with memory impairment, it is recommended to maintain a regular sleep schedule and moderate mental activity, and engage in memory training such as memorization and note taking. Eating foods rich in omega-3 fatty acids can be increased to avoid excessive alcohol consumption. Family members should provide full understanding and support to help patients establish a memory assistance system. Regularly follow up and evaluate changes in cognitive function, and adjust treatment plans if necessary. Early identification and intervention of memory impairment are crucial for improving prognosis.








Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!