A high neutrophil count usually indicates the presence of inflammatory reactions, infections, or stress states in the body, mainly related to bacterial infections, tissue damage, vigorous exercise, drug effects, and blood system diseases.

1. Bacterial infection:
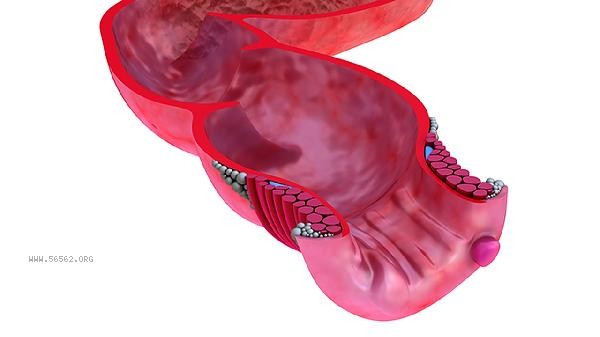
Neutrophils are the main immune cells that resist bacterial infections. When bacterial infections such as pneumonia, urinary tract infections, appendicitis, etc. occur, the bone marrow accelerates the release of neutrophils into the bloodstream, leading to an increase in counts. Clinically, it is often accompanied by symptoms such as fever and local redness and swelling, and the infection site needs to be identified through blood culture or imaging examination.
2. Tissue damage:
Tissue damage caused by trauma, surgery, burns, etc. can trigger inflammatory reactions, promoting the migration of neutrophils to the damaged area. At this point, the increase in count is a physiological defense mechanism, usually accompanied by an increase in C-reactive protein. After injury repair, the value can gradually return to normal. 3. Intense exercise: During high-intensity exercise, adrenaline secretion increases, which mobilizes neutrophils in the marginal pool to enter the circulating blood, causing a transient elevation. This physiological change can recover on its own after 2-4 hours of rest and does not require special treatment.
4. Drug effects:

Corticosteroid drugs such as prednisone can stimulate bone marrow hematopoietic function, leading to neutrophil proliferation. Some antiepileptic drugs and lithium supplements may also cause similar reactions. After discontinuing the medication, the blood count is usually reversible, and regular monitoring of blood routine is required during the medication period.
5. Hematological disorders:
Chronic myeloid leukemia, bone marrow proliferative tumors, and other diseases can lead to abnormal proliferation of neutrophils, often accompanied by sustained elevation and an increase in immature granulocytes. Further differentiation is required through bone marrow puncture and genetic testing, and such situations require specialized intervention in hematology. When high levels of neutrophils are found, it is recommended to recheck the blood routine to rule out detection errors. If there are persistent abnormalities, it is necessary to improve inflammation indicators, peripheral blood smears, and other tests. Overexertion should be avoided in daily life, adequate sleep should be ensured, and appropriate supplementation of vitamin C and protein should be taken to support immune function. During the acute infection period, medication should be taken according to medical advice. For those with chronic elevation, it is recommended to follow up on blood count changes every 3-6 months to avoid factors that worsen inflammation such as smoking and alcohol abuse. If accompanied by persistent fever, weight loss, or lymph node enlargement, timely screening for hematological diseases should be conducted.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!