Elevated levels of eosinophils may be caused by allergic reactions, chronic inflammation, myeloproliferative disorders, endocrine disorders, or drug factors. Eosinophils are a type of white blood cell, and an increase in their proportion usually indicates an abnormal immune response or pathological state in the body.
1. Allergic reactions:
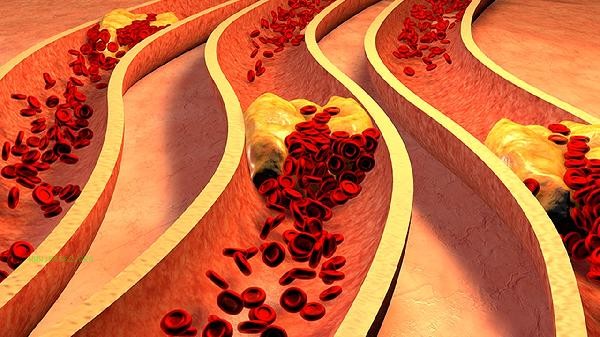
When exposed to allergens such as pollen, dust mites, or specific foods, eosinophils release mediators such as histamine to participate in the allergic reaction. Commonly seen in diseases such as allergic rhinitis and urticaria, blood tests show a mild increase in absolute or percentage of eosinophils, usually accompanied by symptoms such as skin itching and sneezing. 2. Chronic inflammation: Chronic inflammatory diseases such as rheumatoid arthritis and ulcerative colitis can stimulate bone marrow hematopoietic function, leading to compensatory increase in eosinophils. This type of situation is often accompanied by abnormal inflammatory indicators such as increased erythrocyte sedimentation rate and elevated C-reactive protein, which need to be comprehensively judged based on clinical symptoms.
3. Bone marrow proliferative diseases:
Bone marrow abnormal proliferative diseases such as polycythemia vera and chronic myeloid leukemia can cause a significant increase in eosinophils. This type of disease may be accompanied by systemic symptoms such as splenomegaly, night sweats, and weight loss, and should be diagnosed through bone marrow aspiration and genetic testing.
4. Endocrine disorders:
Endocrine diseases such as hypothyroidism and diabetes may affect the hematopoietic microenvironment, leading to a slight increase in basophils. This type of situation is usually accompanied by typical endocrine symptoms such as a decrease in basal metabolic rate and fluctuations in blood sugar, and relevant hormone testing can assist in diagnosis.
5. Drug factors:
Long term use of estrogen preparations, glucocorticoids, or certain antibiotics may interfere with bone marrow hematopoietic function, causing transient elevation of eosinophils. After discontinuing medication, the values can often return to normal, and regular monitoring of blood routine changes is necessary during medication. When high levels of eosinophils are found, a comprehensive evaluation should be conducted in conjunction with other blood routine indicators and clinical symptoms. It is recommended to avoid contact with known allergens, maintain a regular schedule and balanced diet, and supplement with vitamin C and Omega-3 fatty acids in moderation to help regulate immunity. Persistent abnormalities require allergen screening, bone marrow examination, or endocrine function assessment, and an individualized intervention plan will be developed by a specialist doctor. Pay attention to daily observation of accompanying symptoms such as bleeding tendency of skin and mucous membranes, unexplained fever, etc., and regularly check the dynamic monitoring changes of blood routine.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!