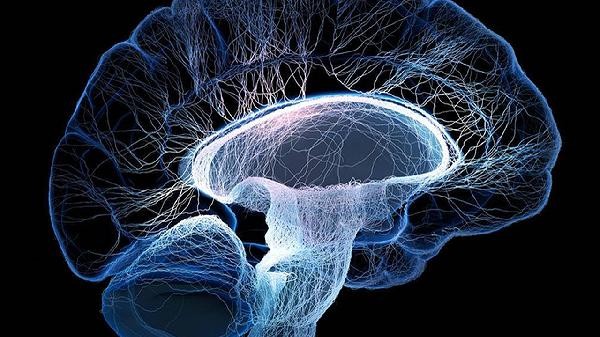
Obsessive compulsive disorder is not simply caused by damage to specific areas of the brain, but is related to abnormal activity and neurotransmitter imbalance in multiple functional areas of the brain. It mainly involves functional disorders in brain areas such as the prefrontal cortex, basal ganglia, and cingulate gyrus, and is also associated with neurotransmitter disorders such as serotonin and dopamine.

1. Functional abnormalities in the prefrontal cortex
The prefrontal cortex is responsible for decision control and behavioral inhibition, and excessive activity in this area may lead to recurrent invasive thinking. Patients often exhibit an inability to suppress unnecessary thoughts and need to alleviate anxiety through repetitive behaviors. Cognitive behavioral therapy can help improve symptoms by regulating prefrontal activity.
2. Dysregulation of basal ganglia circuit
The basal ganglia are associated with habit formation and action execution, and abnormalities in this area can transform simple behaviors into ritualized actions. Abnormal signal transmission in the cerebral cortex basal ganglia thalamus circuit may lead patients to fall into a cycle of compulsive behaviors such as repeated examinations and cleaning.
3. Overactivation of the cingulate gyrus
As an emotional regulatory center, abnormal activity in the cingulate gyrus can amplify false perceptions and threat assessments. Functional imaging shows that patients with obsessive-compulsive disorder have significantly increased activation of the cingulate cortex during task execution, which may exacerbate excessive attention to potential dangers.
Fourth, disorder of serotonin system
Decreased serotonin concentration can affect the efficiency of neural signal transduction, and selective serotonin reuptake inhibitors can alleviate symptoms by regulating synaptic cleft serotonin levels. Some patients have serotonin transporter gene polymorphism, which may increase the risk of disease.
V. Imbalance of Dopamine Pathway
Excessive dopamine release may enhance the reward effect of compulsive behavior, leading to a pathological cycle of repetitive behavior. Some antipsychotic drugs are effective in treating refractory obsessive-compulsive disorder by regulating dopamine receptors, suggesting the role of the dopamine system in symptom maintenance. The neural mechanism of obsessive-compulsive disorder involves the coordinated abnormality of multiple functional networks in the brain. It is recommended that patients combine medication treatment and psychological intervention under professional guidance. Regular sleep patterns and mindfulness training can help alleviate symptoms, avoid excessive fatigue and stress stimuli. Early identification and systematic treatment can significantly improve prognosis, and family members should provide full understanding and support, and cooperate with doctors to develop personalized rehabilitation plans.





Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!