The weight gain after dialysis may be related to water retention, excessive nutrition intake, inadequate dialysis, drug side effects, cardiac dysfunction and other factors. Dialysis patients need to strictly monitor weight changes and adjust treatment plans in a timely manner.

1. Water retention
The renal function of dialysis patients is damaged, which leads to water excretion disorder. Excessive drinking water or high salt diet between two dialysis sessions is easy to cause fluid retention. Symptoms include lower limb edema, elevated blood pressure, and difficulty breathing. It is recommended to weigh and control fluid intake daily, and the weight gain between two dialysis sessions should not exceed 5% of dry weight. Restricting sodium intake can help reduce thirst.
2. Excessive nutrient intake
Some patients have improved appetite after dialysis but have not adjusted their dietary structure. Excessive intake of high calorie foods may lead to fat accumulation. Dialysis consumes protein, but excessive supplementation may be converted into fat storage. It is recommended to maintain a daily intake of around 1.2 grams of protein per kilogram of body weight, prioritize high-quality protein such as fish, eggs, and milk, and avoid fried foods and sweets.
3. Insufficient dialysis
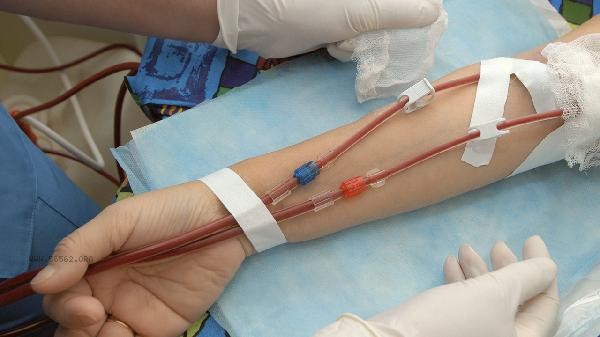
Insufficient dialysis time or inadequate blood flow can lead to incomplete clearance of metabolic waste, causing changes in osmotic pressure in the body and promoting water retention. False weight gain may occur when the urea clearance rate does not meet the standard. It is necessary to regularly evaluate the KT/V value, adjust the dialysis prescription, and ensure at least 12 hours of effective dialysis time per week.
4. Drug side effects
Some antihypertensive drugs such as calcium channel blockers may cause water and sodium retention, and glucocorticoids may promote fat redistribution. Insulin therapy may accelerate fat synthesis due to increased food intake after dialysis. The medication plan should be dynamically adjusted by a nephrologist based on changes in dry weight to avoid the use of drugs that increase fluid load.
5. Cardiac dysfunction
Long term uremia may lead to myocardial lesions, decreased cardiac pumping function, and circulatory congestion. Manifesting as paroxysmal nocturnal dyspnea, jugular vein engorgement, and other symptoms. Cardiac function needs to be evaluated through echocardiography, and diuretics or cardiac stimulants may be used if necessary. Control the amount of dialysis dehydration to avoid excessive dehydration that increases the burden on the heart in a short period of time.

Dialysis patients should establish standardized weight monitoring records, including daily morning fasting weight and pre - and post dialysis weight. We adopt the principle of low salt and high-quality protein in our diet, and our daily liquid intake is 500 milliliters of the previous day's urine output. Choose low-intensity aerobic activities such as walking and Tai Chi for exercise, and avoid intense exercise that can increase the burden on the heart. Regularly review nutritional indicators such as hemoglobin and albumin, and communicate with the dialysis team in a timely manner about any abnormal weight changes. If weight gain exceeds 10% of dry weight or significant edema occurs in the short term, immediate medical attention should be sought to rule out acute complications.









Comments (0)
Leave a Comment
No comments yet
Be the first to share your thoughts!